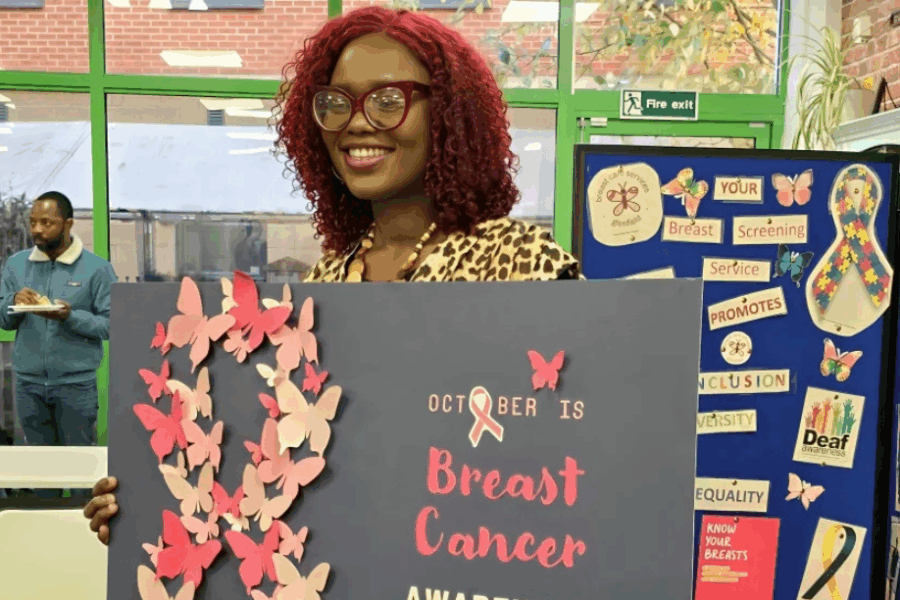
Dr Olubukola Ayodele, a Consultant Medical Oncologist at the University Hospitals of Leicester NHS Trust, has received a £166,965 award from Breast Cancer Now. This funding will be used to investigate how different groups of people experience secondary breast cancer treatments.
The study hopes to transform secondary breast cancer care. It will explore how people with incurable secondary (or metastatic) breast cancer experience treatment side effects. It also aims to find out whether personalised drug doses could help to improve people’s quality of life.
At the moment, an estimated 61,000 people are living with secondary breast cancer in the UK. When breast cancer cells spread from the primary cancer in the breast to other parts of the body, it is called secondary or metastatic breast cancer. Although treatable, it can’t be cured.
Treatments for the disease can cause a wide range of side effects that may significantly impact day-to-day life. Factors such as ethnicity, genetics, and other personal characteristics can influence how individuals experience treatment. This includes side-effects and benefits from cancer therapies. However, there is currently limited understanding of how these experiences differ. This is particularly the case among women from ethnically diverse backgrounds, as many were not included in the initial clinical trials for which these therapies have been licensed.
Finding the right medication dose for each person can be complex, as individuals may respond differently to the same treatment. To better understand this, the research team will conduct a national survey of around 1,000 people living with secondary breast cancer. The survey will explore people’s experiences of finding the most suitable medication dose for them. This will include asking whether they have discussed it with their treatment team, and whether they feel their treatment is tailored to their needs.
Participants will be asked about any challenges they have faced during treatment, such as side effects or difficulty accessing care. The researchers will assess how these experiences may differ for people from ethnically diverse backgrounds.
The team will also hold focus groups to gain deeper insight into the perspectives of people living with secondary breast cancer. The findings will be used to develop recommendations for health professionals on how to better support personalised drug dosing and deliver more effective, patient-centred care. The research will help find ways to make sure that treatments are as effective and gentle as possible for everyone.
Dr Ayodele hopes to build on this work in the future, including exploring clinicians’ perspectives to dose reduction. She said:
“While advances in breast cancer treatment have improved survival rates, there are still significant differences in how people experience these treatments. This is especially true for women from different ethnic backgrounds, who may experience varying side effects and treatment outcomes because of the lack of diversity in clinical trials. Understanding these differences is crucial for ensuring all women receive the best care possible.”
Dr Simon Vincent, Chief Scientific Officer at Breast Cancer Now, said:
“People living with secondary breast cancer deserve treatments that not only work but also allow them to live as fully as possible. By exploring the unique needs of people living with secondary breast cancer, the burden of treatment side effects and identifying opportunities to personalise drug doses, this research could improve the quality of life for patients by tailoring their treatment even more closely to what they need.”
Lydia Chatfield is 31 and from the Midlands. She was diagnosed with primary breast cancer in March 2023, when she was 28. Just two days after Christmas in December 2024, she was told she had secondary breast cancer after a scan revealed tumours in her brain.
Throughout her treatment, Lydia has experienced severe side effects, including headaches, sickness and fatigue. As a mum to two children aged 4 and 7, this has also had a significant impact on what she is able to do with them.
Lydia says: “I’m on a targeted therapy called Kadcyla, which causes nausea and exhaustion. I have to take anti-sickness tablets for three days, and the headaches last for around five days. I had an eight-week break over the summer because I couldn’t do anything with the children otherwise. My youngest has started school now so in the day I can rest. I’m fortunate that I’m able to be at home. The steroids I’m on also make you really irritable, hungry, and wide awake, but then the treatment makes you really tired.
“I don’t want to be knocked down every three weeks when I have treatment. Everyone experiences side effects differently, but you know your body better than anyone. It’s important to speak to your treatment team about the side effects you’re experiencing, because the same thing isn’t going to work for everyone. My side effects are better managed now as I’ve had the confidence to speak up and ask for help.”
Lydia has also undergone stereotactic radio surgery on her brain. She will be having this again after two new tumours were found. Because of her brain treatment, she has been unable to drive since January. She relies on family support to get to appointments and help with the children. She added:
“Research like this is so important. If a dose could be reduced and still have the same positive effect, it might mean I don’t have to struggle or feel so sick, and that our routine wouldn’t have to be disrupted as much as it is when I have treatment. I often want to make plans, but I have to factor in how I’m going feel after treatment. Research like this could change that.”